 By Liliana Cote de Bejarano MD, MPH, CFCP
By Liliana Cote de Bejarano MD, MPH, CFCP
What is “emergency contraception”?
Emergency contraception (EC) is the use of pills or devices after sex to try to prevent pregnancy.1 EC is promoted when a woman has been raped, when a couple has chosen to have sex without using any form of contraception, or when there is a suspected contraceptive failure. Types of EC may include pills or the insertion of the Copper-T Intrauterine Device (IUD) up to five days after intercourse. The use of other drugs as emergency contraception is under investigation.2
What is the “Morning After Pill”?
The phrase “Morning After Pill” (MAP) describes a set of contraceptive pills taken after a sexual act, to prevent pregnancy. One type of MAP contains only the synthetic progestin levonorgestrel (LNG), which is the main drug in other commercial contraceptives. Commercial names for the MAP include Plan B One Step, Take Action, Next Choice One Dose, My Way, and others.3 The Food and Drug Administration has approved Plan B One Step for sale without age restrictions. A second type of MAP is the anti-progesterone “Ella”, available with prescription in the United States. A third type of MAP is the “off label” use of combined oral contraceptive pills. A fourth type of EC is the abortion pill Mifepristone (RU 486), used outside the USA.
How does the Morning After Pill work?
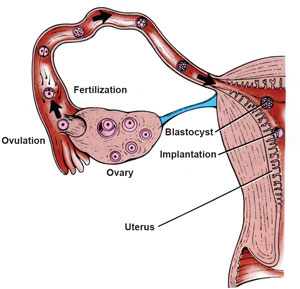
The new baby (blastocyst) migrates from the fallopian tube to the uterus where it implants 5-7 days after conception.
Conception of a new human being is possible only during a few days in the woman’s cycle. Sperm can survive in the woman’s body 3-5 days, and the ovum dies 12-24 hours after ovulation. Fertilization normally occurs in the fallopian tube after ovulation. The new human being (blastocyst) moves from the fallopian tube to the uterus where it implants 5-7 days after conception. A delicate hormonal balance is necessary for the baby’s survival.
Some studies seem to show that Plan B works by changing the cervical mucus or by attacking sperm. More recent studies, however, show that these effects may happen when the drug is taken regularly (like birth control pills), but NOT after one dose (like EC).4,5
Advocates of EC claim that the active ingredient in Plan B works mainly by stopping or delaying ovulation Available studies show that when Plan B was given to women in the fertile part of their cycle, 80% OR MORE of them ovulated, although NONE of them became obviously pregnant (see diagram below).6,7 If sperm and an egg are present in the woman’s body but no obvious pregnancy develops, then abortion is the most likely cause.8 Some studies also show that Plan B disturbs the hormonal balance needed to maintain pregnancy.9,10
What about other types of emergency contraception?
Copper-T IUDs—Copper ions released from an IUD are toxic for sperm and the ovum, decreasing the probability of fertilization.11 Also, the Copper-T IUD lowers the chances of survival of any embryo that may be formed before it reaches the womb. The Copper-T IUD stops the lining of the womb from accepting a newly formed embryo.12 Thus the Copper-T IUD may have a post-fertilization effect, meaning it destroys a young human embryo.
Ella and Mifepristone (RU-486) change the body’s ability to react to some hormones. They can block the action of the hormone progesterone,13 thereby destroying a new human life through chemical abortion. Ella can also delay or block ovulation if taken before ovulation.14
If conception (fertilization) has already taken place, then the only way the IUD and the morning after pill (MAP) can be effective is by destroying the new life. When a woman takes theses pills or when the IUD is inserted, there is currently no way for her or her doctor to know whether or not she has already conceived. A pregnancy test cannot give this information before implantation. Whenever these pills are taken, or a Copper-T IUD is inserted after sexual activity, there is the risk that a new human life will be destroyed.

Remember that
a new life is
destroyed
when implantation
is prevented.
Does this mean that emergency contraception is an abortifacient— that it can cause an abortion?
A new human life begins at conception, also called fertilization. However, in September 1965, the American College of Obstetricians and Gynecologists (ACOG) attempted to redefine “pregnancy” as beginning at the time of implantation, and not at the time of conception. The effectiveness of pills and devices that do not prevent fertilization depends on destruction of a new human life. This should be called an “abortion” in spite of the medical definition from the ACOG.
In a recent study 8 out of 10 women who took the MAP ovulated. This means that if they had sex, some of these 8 women likely became pregnant. None had an obvious pregnancy, so the women who became pregnant probably experienced an early abortion.
How effective is emergency contraception?
The Copper-T IUD prevents 99% of expected pregnancies. Ella and Plan B prevent some of expected pregnancies after unprotected intercourse.15 The effect of EC in reducing unintended pregnancies and induced abortions has not yet been proven. Available studies show that EC may have no effect on unintended pregnancies, it may even increase them.16, 17, 18,19 Women with high body mass may also find that EC has decreased or no effectiveness in preventing pregnancy.20 In addition, providing emergency contraception in advance has the negative effect of increasing risky sexual behavior.21 Overall, the evidence suggests that the Morning After Pill is not effective for preventing unintended pregnancies.
How safe is emergency contraception?
A Morning After Pill that contains LNG can cause heavier or lighter menstrual bleeding, nausea, vomiting, abdominal pain, fatigue, headache, dizziness, breast tenderness, delay of menses (up to 7 days), and diarrhea. The use of LNG also increases the risk of ectopic pregnancy.22 The use of Ella has been connected with headache, abdominal or upper abdominal pain, nausea, dysmenorrhea, fatigue, and dizziness.23 Women who use the Copper-T IUD can experience uterine cramps and other undesirable effects such as ectopic pregnancy, septic abortion, pelvic infection, perforation, embedment, anemia, backache, painful periods, pain during intercourse, vaginal discharges, prolonged menstrual flow, menstrual spotting, cramping, and vaginitis.24
One study reported that women may repeatedly use EC due to an exaggerated perception of its effectiveness.25 Another study found that over-the-counter access to EC leads to increased Sexually Transmitted Infections by approximately 12% for women ages 15-44 due to increased risky sexual behavior.26 More time and research are needed to know the long-term effects of emergency contraception on the health and safety of women.
Are there other options?
If you are single, the surest way to avoid pregnancy or a sexually transmitted infection is abstinence, and it always works. If you are married, the modern methods of Natural Family Planning (NFP) are the safest, healthiest, least toxic, and least expensive means for family planning. Victims of rape or sexual abuse need and deserve the best medical care and human support possible. The additional stress and health risks of emergency contraception add further harm. (Pregnancy due to rape is estimated at 5%).27 For the vast majority of these women, emergency contraceptives impose significant health risks with no benefit. If conception has already occurred, then a very early abortion is the only means for emergency contraception to be effective. Abortion carries with it many serious adverse consequences such as increased rates of breast cancer, depression, anxiety, suicidal behaviors, and substance use disorders.28 A far safer approach is to carry the child to term. Adoption is always an option.
Confidential pregnancy assistance services are available throughout the U.S. and Canada by calling Option Line at 800-395-HELP (4357) and Abortion Pill Reversal Network at 877-558-0333.
REFERENCES:
1. Trussell J, PhD and Raymond, EG, MD, MPH. Emergency contraception: a last chance to prevent unintended pregnancy. Retrieved from: http://ec.princeton.edu/questions/ec-review.pdf, July 28 2015.
2. Jesam C, Salvatierra AM, Schwartz JL, & Croxatto HB. (2010). Suppression of follicular rupture with meloxicam, a cyclooxygenase-2 inhibitor: Potential for emergency contraception. Human Reproduction (Oxford, England), 25(2), 368-373.
3. Emergency Contraception Pills. Retrieved from http://ec.princeton.edu/info/ecp.html, July 28 2015.
4. Nascimento JA, Seppala M, Perdigao A., Espejo-Arce X, Munuce MJ, Hautala L, et al. (2007). In vivo assessment of the human sperm acrosome reaction and the expression of glycodelin-A in human endometrium after levonorgestrel-emergency contraceptive pill administration. Human Reproduction (Oxford, England), 22(8), 2190-2195.
5. Hermanny A, Bahamondes MV, Fazano F, Marchi NM, Ortiz ME, Genghini MH, et al. (2012). In vitro assessment of some sperm function following exposure to levonorgestrel in human fallopian tubes. Reproductive Biology and Endocrinology : RB&E, 10, 8-7827-10-8.
6. Brache V, Cochon L, Deniaud M, Croxatto, HB. Ulipristal acetate prevents ovulation more effectively than levonorgestrel: analysis of pooled data from three randomized trials of emergency contraception regimens. Contraception. Nov 2013; 88(5): 611-618.
7. Noe G, Croxatto HB, Salvatierra AM, Reyes V, Villarroel C, Munoz C, et al. Contraceptive efficacy of emergency contraception with levonorgestrel given before or after ovulation. Contraception. Nov 2011; 84(5): 486-492.
8. Kahlenborn C, Peck R, & Severs WB. (2015). Mechanism of action of levonorgestrel emergency contraception. The Linacre Quarterly, 82(1), 18-33.
9. Croxatto HB, Brache V, Pavez M, Cochon L, Forcelledo ML, Alvarez F, et al. Pituitary-ovarian function following the standard levonorgestrel emergency contraceptive dose or a single 0.75-mg dose given on the days preceding ovulation. Contraception. Dec 2004; 70(6): 442-450.
10. Hapangama D, Glasier AF, Baird DT. The effects of peri-ovulatory administration of levonorgestrel on the menstrual cycle. Contraception. Mar 2001; 63(3): 123-129.
11. Ortiz ME, Croxatto HB. Copper-T intrauterine device and levonorgestrel intrauterine system: biological bases of their mechanism of action. Contraception. Jun 2007; 75(6 Suppl): S16-30.
12. Gemzell-Danielsson K, Berger C & Lalitkumar PGL. (2013). Emergency contraception–mechanisms of action. Contraception, 87(3), 300-308.
13. Keenan JA. Ulipristal acetate: contraceptive or contragestive? Ann Pharmacother. Jun 2011; 45(6): 813-815.
14. Brache V, Cochon L, Jesam C, Maldonado R, Salvatierra AM, Levy DP, et al. Immediate pre-ovulatory administration of 30 mg ulipristal acetate significantly delays follicular rupture. Hum Reprod. Sep 2010; 25(9): 2256-2263.
15. Fred F. Ferri M.D., F.A.C.P. (2016). Ferri’s clinical advisor 2016 Elsevier, Inc
16. Rodriguez MI, Curtis KM, Gaffield ML, Jackson E, Kapp N. Advance supply of emergency contraception: a systematic review. Contraception. May 2013; 87(5): 590-601.
17. Raymond EG, Trussell J, Polis CB. Population effect of increased access to emergency contraceptive pills: a systematic review. Obstet Gynecol. January 2007; 109(1): 181-188.
18. Walsh TL, Frezieres RG. Patterns of emergency contraception use by age and ethnicity from a randomized trial comparing advance provision and information only. Contraception. Aug 2006; 74(2): 110-117.
19. Glasier A, Fairhurst K, Wyke S, Ziebland S, Seaman P, Walker J, et al. Advanced provision of emergency contraception does not reduce abortion rates. Contraception. May 2004; 69(5): 361-366.
20. Glasier A, Cameron ST, Blithe D, Scherrer B, Mathe H, Levy D, et al. (2011). Can we identify women at risk of pregnancy despite using emergency contraception? data from randomized trials of ulipristal acetate and levonorgestrel. Contraception, 84(4), 363-367.
21. Belzer M, Sanchez K, Olson J, Jacobs AM, Tucker D. Advance supply of emergency contraception: a randomized trial in adolescent mothers. J Pediatr Adolesc Gynecol. Oct 2005; 18(5): 347-354.
22. Zhang J, Li C, Zhao WH. Xi X, Cao SJ, Ping H, et al. (2015). Association between levonorgestrel emergency contraception and the risk of ectopic pregnancy: A multicenter case-control study. Scientific Reports, 5, 8487.
23. Ulipristal Acetate. http://www.pdr.net/drug-summary/ella?druglabelid=1278 August 10 2015
24. Intrauterine Copper Contraceptive Paragard. Retrieved from http://www.pdr.net/drug-summary/paragard?druglabelid=572 August 10 2015
25. Melton L, Stanford JB, Dewitt MJ. Use of levonorgestrel emergency contraception in Utah: is it more than “plan B”? Perspect Sex Reprod Health. Mar 2012; 44(1): 22-29.
26. Mulligan K. (2015). Access to emergency contraception and its impact on fertility and sexual behavior. Health Economics (Published Online).
27. Holmes MM, Resnick HS, Kilpatrick DG, Best CL. Rape-related pregnancy: estimates and descriptive characteristics from a national sample of women. Am J Obstet Gynecol. August 1996; 175(2): 320-324.
28. Fergusson DM, Horwood LJ, Ridder EM. Abortion in young women and subsequent mental health. J Child Psychol Psych. January 2006; 47(1): 16-24.
Sorry, This product is currently unavailable
This entry was posted
on Tuesday, March 19th, 2013 at 12:21 am and is filed under Featured, News & Commentary, Publications.
You can follow any responses to this entry through the RSS 2.0 feed.
You can leave a response, or trackback from your own site.
The Morning After Pill and other types of “Emergency Contraception”–Myths and Realities
What is “emergency contraception”?
Emergency contraception (EC) is the use of pills or devices after sex to try to prevent pregnancy.1 EC is promoted when a woman has been raped, when a couple has chosen to have sex without using any form of contraception, or when there is a suspected contraceptive failure. Types of EC may include pills or the insertion of the Copper-T Intrauterine Device (IUD) up to five days after intercourse. The use of other drugs as emergency contraception is under investigation.2
What is the “Morning After Pill”?
The phrase “Morning After Pill” (MAP) describes a set of contraceptive pills taken after a sexual act, to prevent pregnancy. One type of MAP contains only the synthetic progestin levonorgestrel (LNG), which is the main drug in other commercial contraceptives. Commercial names for the MAP include Plan B One Step, Take Action, Next Choice One Dose, My Way, and others.3 The Food and Drug Administration has approved Plan B One Step for sale without age restrictions. A second type of MAP is the anti-progesterone “Ella”, available with prescription in the United States. A third type of MAP is the “off label” use of combined oral contraceptive pills. A fourth type of EC is the abortion pill Mifepristone (RU 486), used outside the USA.
How does the Morning After Pill work?
The new baby (blastocyst) migrates from the fallopian tube to the uterus where it implants 5-7 days after conception.
Conception of a new human being is possible only during a few days in the woman’s cycle. Sperm can survive in the woman’s body 3-5 days, and the ovum dies 12-24 hours after ovulation. Fertilization normally occurs in the fallopian tube after ovulation. The new human being (blastocyst) moves from the fallopian tube to the uterus where it implants 5-7 days after conception. A delicate hormonal balance is necessary for the baby’s survival.
Some studies seem to show that Plan B works by changing the cervical mucus or by attacking sperm. More recent studies, however, show that these effects may happen when the drug is taken regularly (like birth control pills), but NOT after one dose (like EC).4,5
Advocates of EC claim that the active ingredient in Plan B works mainly by stopping or delaying ovulation Available studies show that when Plan B was given to women in the fertile part of their cycle, 80% OR MORE of them ovulated, although NONE of them became obviously pregnant (see diagram below).6,7 If sperm and an egg are present in the woman’s body but no obvious pregnancy develops, then abortion is the most likely cause.8 Some studies also show that Plan B disturbs the hormonal balance needed to maintain pregnancy.9,10
What about other types of emergency contraception?
Copper-T IUDs—Copper ions released from an IUD are toxic for sperm and the ovum, decreasing the probability of fertilization.11 Also, the Copper-T IUD lowers the chances of survival of any embryo that may be formed before it reaches the womb. The Copper-T IUD stops the lining of the womb from accepting a newly formed embryo.12 Thus the Copper-T IUD may have a post-fertilization effect, meaning it destroys a young human embryo.
Ella and Mifepristone (RU-486) change the body’s ability to react to some hormones. They can block the action of the hormone progesterone,13 thereby destroying a new human life through chemical abortion. Ella can also delay or block ovulation if taken before ovulation.14
If conception (fertilization) has already taken place, then the only way the IUD and the morning after pill (MAP) can be effective is by destroying the new life. When a woman takes theses pills or when the IUD is inserted, there is currently no way for her or her doctor to know whether or not she has already conceived. A pregnancy test cannot give this information before implantation. Whenever these pills are taken, or a Copper-T IUD is inserted after sexual activity, there is the risk that a new human life will be destroyed.
Remember that
a new life is
destroyed
when implantation
is prevented.
Does this mean that emergency contraception is an abortifacient— that it can cause an abortion?
A new human life begins at conception, also called fertilization. However, in September 1965, the American College of Obstetricians and Gynecologists (ACOG) attempted to redefine “pregnancy” as beginning at the time of implantation, and not at the time of conception. The effectiveness of pills and devices that do not prevent fertilization depends on destruction of a new human life. This should be called an “abortion” in spite of the medical definition from the ACOG.
How effective is emergency contraception?
The Copper-T IUD prevents 99% of expected pregnancies. Ella and Plan B prevent some of expected pregnancies after unprotected intercourse.15 The effect of EC in reducing unintended pregnancies and induced abortions has not yet been proven. Available studies show that EC may have no effect on unintended pregnancies, it may even increase them.16, 17, 18,19 Women with high body mass may also find that EC has decreased or no effectiveness in preventing pregnancy.20 In addition, providing emergency contraception in advance has the negative effect of increasing risky sexual behavior.21 Overall, the evidence suggests that the Morning After Pill is not effective for preventing unintended pregnancies.
How safe is emergency contraception?
A Morning After Pill that contains LNG can cause heavier or lighter menstrual bleeding, nausea, vomiting, abdominal pain, fatigue, headache, dizziness, breast tenderness, delay of menses (up to 7 days), and diarrhea. The use of LNG also increases the risk of ectopic pregnancy.22 The use of Ella has been connected with headache, abdominal or upper abdominal pain, nausea, dysmenorrhea, fatigue, and dizziness.23 Women who use the Copper-T IUD can experience uterine cramps and other undesirable effects such as ectopic pregnancy, septic abortion, pelvic infection, perforation, embedment, anemia, backache, painful periods, pain during intercourse, vaginal discharges, prolonged menstrual flow, menstrual spotting, cramping, and vaginitis.24
One study reported that women may repeatedly use EC due to an exaggerated perception of its effectiveness.25 Another study found that over-the-counter access to EC leads to increased Sexually Transmitted Infections by approximately 12% for women ages 15-44 due to increased risky sexual behavior.26 More time and research are needed to know the long-term effects of emergency contraception on the health and safety of women.
Are there other options?
If you are single, the surest way to avoid pregnancy or a sexually transmitted infection is abstinence, and it always works. If you are married, the modern methods of Natural Family Planning (NFP) are the safest, healthiest, least toxic, and least expensive means for family planning. Victims of rape or sexual abuse need and deserve the best medical care and human support possible. The additional stress and health risks of emergency contraception add further harm. (Pregnancy due to rape is estimated at 5%).27 For the vast majority of these women, emergency contraceptives impose significant health risks with no benefit. If conception has already occurred, then a very early abortion is the only means for emergency contraception to be effective. Abortion carries with it many serious adverse consequences such as increased rates of breast cancer, depression, anxiety, suicidal behaviors, and substance use disorders.28 A far safer approach is to carry the child to term. Adoption is always an option.
Confidential pregnancy assistance services are available throughout the U.S. and Canada by calling Option Line at 800-395-HELP (4357) and Abortion Pill Reversal Network at 877-558-0333.
REFERENCES:
1. Trussell J, PhD and Raymond, EG, MD, MPH. Emergency contraception: a last chance to prevent unintended pregnancy. Retrieved from: http://ec.princeton.edu/questions/ec-review.pdf, July 28 2015.
2. Jesam C, Salvatierra AM, Schwartz JL, & Croxatto HB. (2010). Suppression of follicular rupture with meloxicam, a cyclooxygenase-2 inhibitor: Potential for emergency contraception. Human Reproduction (Oxford, England), 25(2), 368-373.
3. Emergency Contraception Pills. Retrieved from http://ec.princeton.edu/info/ecp.html, July 28 2015.
4. Nascimento JA, Seppala M, Perdigao A., Espejo-Arce X, Munuce MJ, Hautala L, et al. (2007). In vivo assessment of the human sperm acrosome reaction and the expression of glycodelin-A in human endometrium after levonorgestrel-emergency contraceptive pill administration. Human Reproduction (Oxford, England), 22(8), 2190-2195.
5. Hermanny A, Bahamondes MV, Fazano F, Marchi NM, Ortiz ME, Genghini MH, et al. (2012). In vitro assessment of some sperm function following exposure to levonorgestrel in human fallopian tubes. Reproductive Biology and Endocrinology : RB&E, 10, 8-7827-10-8.
6. Brache V, Cochon L, Deniaud M, Croxatto, HB. Ulipristal acetate prevents ovulation more effectively than levonorgestrel: analysis of pooled data from three randomized trials of emergency contraception regimens. Contraception. Nov 2013; 88(5): 611-618.
7. Noe G, Croxatto HB, Salvatierra AM, Reyes V, Villarroel C, Munoz C, et al. Contraceptive efficacy of emergency contraception with levonorgestrel given before or after ovulation. Contraception. Nov 2011; 84(5): 486-492.
8. Kahlenborn C, Peck R, & Severs WB. (2015). Mechanism of action of levonorgestrel emergency contraception. The Linacre Quarterly, 82(1), 18-33.
9. Croxatto HB, Brache V, Pavez M, Cochon L, Forcelledo ML, Alvarez F, et al. Pituitary-ovarian function following the standard levonorgestrel emergency contraceptive dose or a single 0.75-mg dose given on the days preceding ovulation. Contraception. Dec 2004; 70(6): 442-450.
10. Hapangama D, Glasier AF, Baird DT. The effects of peri-ovulatory administration of levonorgestrel on the menstrual cycle. Contraception. Mar 2001; 63(3): 123-129.
11. Ortiz ME, Croxatto HB. Copper-T intrauterine device and levonorgestrel intrauterine system: biological bases of their mechanism of action. Contraception. Jun 2007; 75(6 Suppl): S16-30.
12. Gemzell-Danielsson K, Berger C & Lalitkumar PGL. (2013). Emergency contraception–mechanisms of action. Contraception, 87(3), 300-308.
13. Keenan JA. Ulipristal acetate: contraceptive or contragestive? Ann Pharmacother. Jun 2011; 45(6): 813-815.
14. Brache V, Cochon L, Jesam C, Maldonado R, Salvatierra AM, Levy DP, et al. Immediate pre-ovulatory administration of 30 mg ulipristal acetate significantly delays follicular rupture. Hum Reprod. Sep 2010; 25(9): 2256-2263.
15. Fred F. Ferri M.D., F.A.C.P. (2016). Ferri’s clinical advisor 2016 Elsevier, Inc
16. Rodriguez MI, Curtis KM, Gaffield ML, Jackson E, Kapp N. Advance supply of emergency contraception: a systematic review. Contraception. May 2013; 87(5): 590-601.
17. Raymond EG, Trussell J, Polis CB. Population effect of increased access to emergency contraceptive pills: a systematic review. Obstet Gynecol. January 2007; 109(1): 181-188.
18. Walsh TL, Frezieres RG. Patterns of emergency contraception use by age and ethnicity from a randomized trial comparing advance provision and information only. Contraception. Aug 2006; 74(2): 110-117.
19. Glasier A, Fairhurst K, Wyke S, Ziebland S, Seaman P, Walker J, et al. Advanced provision of emergency contraception does not reduce abortion rates. Contraception. May 2004; 69(5): 361-366.
20. Glasier A, Cameron ST, Blithe D, Scherrer B, Mathe H, Levy D, et al. (2011). Can we identify women at risk of pregnancy despite using emergency contraception? data from randomized trials of ulipristal acetate and levonorgestrel. Contraception, 84(4), 363-367.
21. Belzer M, Sanchez K, Olson J, Jacobs AM, Tucker D. Advance supply of emergency contraception: a randomized trial in adolescent mothers. J Pediatr Adolesc Gynecol. Oct 2005; 18(5): 347-354.
22. Zhang J, Li C, Zhao WH. Xi X, Cao SJ, Ping H, et al. (2015). Association between levonorgestrel emergency contraception and the risk of ectopic pregnancy: A multicenter case-control study. Scientific Reports, 5, 8487.
23. Ulipristal Acetate. http://www.pdr.net/drug-summary/ella?druglabelid=1278 August 10 2015
24. Intrauterine Copper Contraceptive Paragard. Retrieved from http://www.pdr.net/drug-summary/paragard?druglabelid=572 August 10 2015
25. Melton L, Stanford JB, Dewitt MJ. Use of levonorgestrel emergency contraception in Utah: is it more than “plan B”? Perspect Sex Reprod Health. Mar 2012; 44(1): 22-29.
26. Mulligan K. (2015). Access to emergency contraception and its impact on fertility and sexual behavior. Health Economics (Published Online).
27. Holmes MM, Resnick HS, Kilpatrick DG, Best CL. Rape-related pregnancy: estimates and descriptive characteristics from a national sample of women. Am J Obstet Gynecol. August 1996; 175(2): 320-324.
28. Fergusson DM, Horwood LJ, Ridder EM. Abortion in young women and subsequent mental health. J Child Psychol Psych. January 2006; 47(1): 16-24.
Sorry, This product is currently unavailable
This entry was posted on Tuesday, March 19th, 2013 at 12:21 am and is filed under Featured, News & Commentary, Publications. You can follow any responses to this entry through the RSS 2.0 feed. You can leave a response, or trackback from your own site.