Risks & Consequences
Women at High Risk of Significant Bone Loss on Injectable Birth Control Identified
ScienceDaily (Dec. 22, 2009) — Nearly half of women using depot medroxyprogesterone acetate (DMPA), commonly known as the birth control shot, will experience high bone mineral density (BMD) loss in the hip or lower spine within two years of beginning the contraceptive, according to researchers at the University of Texas Medical Branch at Galveston.
The study, reported in the January 2010 issue of Obstetrics and Gynecology, was the first to show that women on DMPA who smoke, have low levels of calcium intake and never gave birth are at the highest risk for BMD loss. The researchers also found that high risk women continued to experience significant losses in BMD during the third year of DMPA use, especially in the hip — the most common facture site in elderly women.
DMPA is an injected contraceptive administered to patients every three months. According to the American College of Obstetricians and Gynecologists, more than two million American women use DMPA, including approximately 400,000 teens. DMPA is relatively inexpensive compared with some other forms of birth control, has a low failure rate and doesn’t need to be administered daily, which contributes to the contraceptive’s popularity. (more…)
What a Woman Should Know about Birth Control
According to the National Survey of Family Growth, between the years 2017-2019, there were 72.7 million women of reproductive age (15–49) using contraception in the United States. The same source reported that oral contraceptive pills were used by over 15 million women. Over 30 million women used other birth control methods, and almost 26 million of these were either sterilized or living with a sterilized man. Long-acting reversible contraception (including the intrauterine device and the Implant) was used by more than 11 million women. Other widely used methods of birth control included condoms (nearly 9 million women), contraceptive injections (2 million), and withdrawal (4 million).1
The Pill consists of one or more types of artificial hormones called estrogens and progestins. It works by inhibiting ovulation and sperm transport and by changing the lining of the inside of a woman’s uterus (called the endometrium) so that implantation of a newly conceived embryo is unlikely.
Ethical Concerns: When the Pill works by preventing implantation of a recently conceived embryo, it produces an early abortion.2
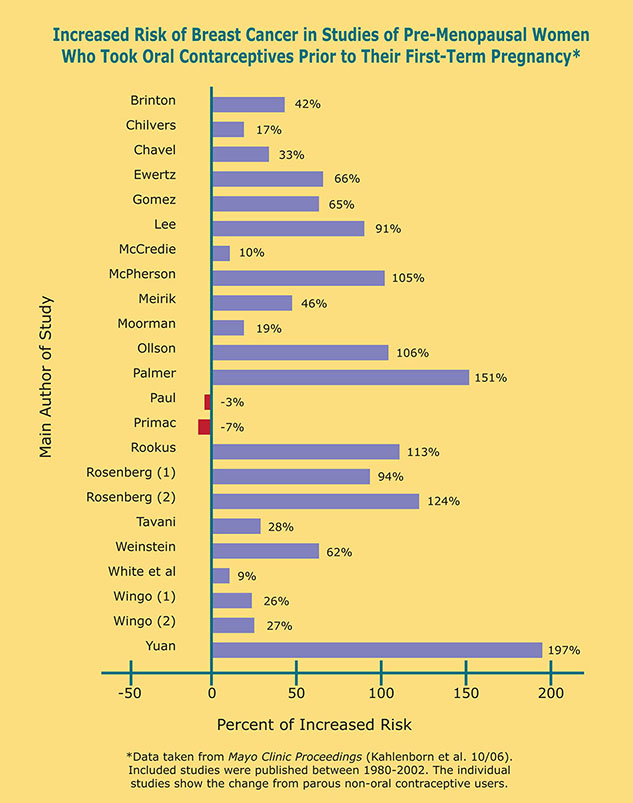
Medical side effects: In 2005, the World Health Organization officially classified oral contraceptives as Group I carcinogens (Group I being the most dangerous from Groups I-IV).3 A year later, a comprehensive meta-analysis published in the Mayo Clinic Proceedings, noted that 21 out of 23 studies found an increased risk of developing premenopausal breast cancer in women who had taken the Pill prior to the birth of their first child. Overall this group of women experienced a 44% increased risk in developing breast cancer prior to age 50.4 Other side effects that women have experienced include high blood pressure, blood clots, strokes, heart attacks, depression, weight gain, and migraines.5 Although the Pill decreases the risk of ovarian and uterine cancer, it increases the risk of breast, liver and cervical cancer.6 At least three studies have noted that the AIDS virus is transmitted more easily to women who are taking the Pill if their partner(s) have the AIDS virus.7,8,9
“The Shot”
Commonly known as “the Shot,” Depo-Provera, a long acting progestin hormone, is injected into a woman’s muscle every three months. It works by decreasing ovulation, by inhibiting sperm transport and by changing the lining of a woman’s uterus.10
Ethical concerns: By changing the lining of the uterus, Depo-Provera can cause an early abortion when conception does occur.
Medical side effects: The results of two major world studies have shown that women who take Depo-Provera for two years or more before age 25 have at least a 190% increased risk of developing breast cancer.11 In addition, Depo-Provera may reduce a woman’s bone density,12 and worsen her cholesterol level.13 One study found that women who had received injectable progestins (i.e., usually Depo-Provera or norethisterone enanthate) for at least five years suffered a 430% increased risk of developing cervical cancer.14 Several studies have shown that women who receive injectable progestins have a much higher rate of contracting the AIDS virus if their partner is infected, with one study showing a 240% increased risk.15
Other Hormonal Contraceptives
The same artificial hormones used in the Pill and Depo-Provera are packaged in a variety of other delivery systems: the Patch, the “Morning after Pill,” hormone impregnated IUDs and vaginal inserts, and others. More are in development. Most are so new that their side effects have not been well researched. They use similar hormones as in the Pill and can be expected to have generally the same cancer-producing risks.
Barrier Methods: The Condom and the Diaphragm
The condom and diaphragm are latex devices used to prevent sperm from reaching the ovum, thus preventing fertilization.
Medical side effects: The condom has a failure rate for avoiding pregnancy that is estimated to be between 10-30%.16, 17 There are several reasons: breakage or slippage during use, manufacturing defects, and defects caused by shipping and storage in a hot or very cold place. A comprehensive review of condom effectiveness in preventing sexually transmitted diseases, sponsored by the US National Institutes of Health, published in 2001, concluded that use of condoms reduces, but does not eliminate transmission of the AIDS virus to men and women and of gonorrhea to men. The review also concluded that condoms have no proven effectiveness in reducing the transmission of any other STD.18 At least one study has noted that women who use barrier methods such as the diaphragm or condom, or the withdrawal method, had a 137% increased risk of developing preeclampsia.19 Preeclampsia, a complication occurring in some pregnant women, is a syndrome of high blood pressure, fluid retention, and kidney damage, which may eventually lead to prolonged seizures and/or coma. It is theorized that exposure to the male’s semen plays a protective role against preeclampsia.
Spermicides
A spermicide is an agent that is designed to kill the man’s sperm and is often sold as a gel or as an ingredient in the vaginal sponge.
Medical side effects: Toxic Shock Syndrome has been associated with the spermicide sponge.20 One researcher has noted that couples who have used certain spermicides within a month of conception have experienced a doubling in the rate of birth defects, as well as a doubling of the rate of miscarriage.21
The IUD (Intrauterine Device)
This is a T-shaped device made of hard plastic. It may also contain copper or progestin hormones. A doctor inserts it into a woman’s uterus. It works by irritating the lining of the uterus and obstructing sperm transport.
Ethical concerns: When conception occurs with an IUD in place, the IUD can prevent implantation, thus causing an early abortion.22
Medical side effects: These include uterine perforation, which may lead to a hysterectomy, and infections, such as a pelvic or tubo-ovarian abscess. Use of all IUDs has been associated with an increased incidence of PID (Pelvic Inflammatory Disease).23 The use of IUDs have been associated with actinomycosis, an infection that can cause long term complications such as pelvic mass and infertility.24 The IUD may occasionally result in pregnancy and if this were to occur, an ectopic pregnancy would be more likely to occur. An ectopic pregnancy is one in which the unborn child implants himself/ herself in a location other than in the mother’s uterus, usually in the Fallopian tube. According to Rossing and Daling, two prominent researchers, women who had used an IUD for three or more years were more than twice as likely to have a tubal pregnancy as women who had never used an IUD, even years after the IUD had been removed.25 Ectopic pregnancy remains the leading cause of maternal death in the United States. The IUD may also cause back aches, cramping, dyspareunia (painful intercourse), dysmenorrhea (painful menstrual cycles), and infertility. 23
“Permanent” Sterilization: Tubal Ligation and Vasectomy
Surgical sterilization attempts to achieve permanent sterility by cutting, burning or tying a woman’s Fallopian tubes (called “tubal ligation”) or a man’s vas deferens (called “vasectomy”). Essure was a permanent non-surgical type of sterilization. Inserts placed in the Fallopian tubes caused a tissue barrier to form that prevented sperm from reaching the egg.
Medical side effects: Tubal ligation does not always prevent conception. When conception does occur, it is associated with a much higher incidence of ectopic pregnancy,26 which, is, as was noted, the leading cause of death in pregnant women. In addition, women who undergo the procedure may experience complications from the anesthesia or from surgery. Complications include bladder puncture, bleeding, and even cardiac arrest after inflation of the abdomen with carbon dioxide.27 Some women who have undergone a tubal ligation experience a syndrome of intermittent vaginal bleeding associated with severe cramping pain in the lower abdomen.28 Essure was discontinued in 2018 due to several adverse events including, perforation of the uterus, improper placement, pain, infection, and nickel allergy.29
About 50% of men who undergo a vasectomy will develop anti-sperm antibodies. In essence, their bodies will come to recognize their own sperm as “the enemy.” This could lead to a higher incidence of autoimmune disease. Several studies have noted that men who undergo a vasectomy have a higher incidence of developing prostate cancer, especially 15-20 years after their vasectomy.30 31,32,33,34 One recent study found an association between vasectomy and aggressive prostate cancer.35 Vasectomy has also been associated with a rare type of dementia.36
Wise Options
The best option before marriage is abstinence. The obvious benefits include greater self-respect, freedom from the risk of sexually transmitted disease, as well as monetary savings and no chance of an unintended pregnancy. Within marriage it should be noted that an openness towards having children yields specific medical benefits. Every additional child a woman bears reduces her risk of breast cancer and ovarian cancer by 5-10%. In addition, breast and ovarian cancer risks are reduced significantly in women who breast feed, with highest reductions in those women who breast-fed for the longest time intervals.37
NFP: Natural Family Planning
Natural Family Planning is a totally natural method by which couples can manage their fertility. In NFP a woman determines when she is either fertile or infertile by observing the consistency of her cervical mucus or other biomarkers such as her temperature. The largest trial to date (about 20,000 Indian women)—sponsored by the WHO (World Health Organization)—found an unintended pregnancy rate of less than 0.2%.38
One obvious benefit of NFP is that there is no increased risk of cancer or other diseases as opposed to hormonal contraceptives. Couples who use NFP have a divorce rate that is less than 5%39—far lower than the national rate of about 50%.
Buy it now:
What a Woman Should Know about Birth Control « One More Soul
REFERENCES:
1. Current Contraceptive Status Among Women Aged 15–49: United States, 2017–2019
Retrieved from: NCHS Data Brief, Number 288, October 2020 (cdc.gov)
2. Larimore WL, Stanford JB. Postfertilization effects of oral contraceptives and their relationship to informed consent. Arch Fam Med. 2000; 9: 126–133.
3. International Agency for Research on Cancer. Combined estrogen-progestogen contraceptives and combined estrogen-progestogen menopausal therapy. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. 2007; Vol 91. available at http://monographs.iarc.fr/ENG/Monographs/vol91/mono91-6E.pdf
4. Kahlenborn C, et al. Oral contraceptive use as a risk factor for premenopausal breast cancer: A meta-analysis. Mayo Clin Proc. 2006 Oct; 81(10): 1290-1302.
5. Kahlenborn C. Breast Cancer, Its Link to Abortion and the Birth Control Pill. Dayton, OH: One More Soul; 2000; 229-231.
6. For overall cancer risk from several cancers due to oral contraceptive use: Kahlenborn C. Breast Cancer, Its Link to Abortion and the Birth Control Pill. Dayton, OH: One More Soul; 2000: 228-229.
7. Allen S, et al. Human immunodeficiency virus infection in urban Rwanda. JAMA. 1991; 266: 1657-1663.
8. Simonsen JN, et al. HIV infection among lower socioeconomic strata prostitutes in Nairobi. AIDS. 1990; Feb: 139-144.
9. Mali JKG, et al. Contraceptive use and the risk of HIV infection in Nairobi, Kenya. Inter J Gynaecol Obstet. 1995; 48(1): 61-67.
10. The Society of Obstetricians and Gynaecologists of Canada. Injection (Depo-Provera). retrieved from http://www.sexualityandu.ca/professionals/contraception-1-3.aspx September 27, 2008.
11. Skegg DCG, et al. Depot medroxyprogesterone acetate and breast cancer: a pooled analysis of the World Health Organization and New Zealand studies. JAMA. 1995; 273(10): 799-804.
12. Wooltorton E. Medroxyprogesterone acetate (Depo-Provera) and bone mineral density loss. CMAJ. 2005; 172(6): 746.
13. Mia AR, et al. Effects of prolonged use of injectable hormonal contraceptive on serum lipid profile. Mymensingh Med J. 2005 Jan; 14(1): 19-21.
14. Herrero R, et al. Injectable contraceptives and risk of invasive cervical cancer: evidence of an association. Int J Cancer. 1990; 46(1): 5-7.
15. Crook AM, Ford D, Gafos M, Hayes R, Kamali A, Kapiga S, et al. Injectable and oral contraceptives and risk of HIV acquisition in women: an analysis of data from the MDP301 trial. Hum Reprod. 2014 Aug; 29(8): 1810-1817.
16. Collart D. Biochemistry & Molecular Biology. Condom failure for protection from sexual transmission of the HIV-a review of the medical literature. 1993, 5393 Whitney Ct., Stone Mountain, GA 30088.
17. Rahwan R. Chemical Contraceptives, Interceptives and Abortifacients. 1995. College of Pharmacy, Ohio State University.
18. National Institute of Allergy and Infectious Diseases. Scientific Evidence on Condom Effectiveness for Sexually Transmitted Disease (STD) Prevention [workshop June 2000], Summary report of the National Institute of Allergy and Infectious Diseases, NIH. DHHS. July 20, 2001.
19. Klonoff-Cohen HS, et al. An epidemiologic study of contraception and preeclampsia. JAMA. 1989 Dec; 262(22): 3143-3147.
20. Faich G, et al. Toxic shock syndrome and the vaginal contraceptive sponge. JAMA. 1986 Jan; 255: 216-218.
21. Jick H, et al. Vaginal spermicides and congenital disorders. JAMA. 1981 Apr; 245(13): 1329-1332.
22. Stanford J MD MSPH. Mechanism of action of intrauterine devices: Update and estimation of post-fertilization effects. Am J Obstet Gynecol. December 2002; 187(6).
23. Bayer HealthCare Pharmaceuticals Inc. Mirena. retrieved from http://www.drugs.com/pro/mirena.html September 27, 2008 and Bayer HealthCare Pharmaceuticals Inc. Paragard. retrieved from http://www.drugs.com/pro/paragard.html September 27, 2008
24. Pillai M, Van de Venne M, Shefras J. Serious morbidity with long-term IUD retention. J Fam Plann Reprod Health Care. 2009 Apr; 35(2): 131-2.
25. Daling J, et al. Past use of an intrauterine device and risk of tubal pregnancy. Epidemiology. 1994; 5:129-130.
26. Gaeta TJ, et al. Atypical ectopic pregnancy. Am J Emerg Med. 1993 May; 11(3): 233-234.
27. Dunn HP. Unexpected Sequelae of Sterilization. International Review of Natural Family Planning, 1:4 (Winter 1977) 318.
28. Townsend DE, et al. Post-ablation-tubal sterilization syndrome. Obstet Gynecol. 1993; 82: 422-424.
29. Essure Permanent Birth Control. Retrieved from: Essure Permanent Birth Control | FDA
30. Rosenberg L, et al. Vasectomy and the risk of prostate cancer. Am J Epidemiol. 1990; 132(6): 1051-1055.
31. Giovannucci E, et al. A prospective cohort study of vasectomy and prostate cancer in US men. JAMA. 1993 Feb; 269(7): 873-877.
32. Giovannucci E, et al. A retrospective cohort study of vasectomy and prostate cancer in US men. JAMA. 1993 Feb; 269: 878-882.
33. Hayes RB, et al. Vasectomy and prostate cancer in US Blacks and Whites. Am J Epidemiol. 1993; 137: 263-269.
34. Rosenberg L, et al. Vasectomy and the risk of prostate cancer. Am J Epidemiol. 1990; 132: 1051-1055.
35. Siddiqui MM, Wilson KM, Epstein MM, Rider JR, Martin NE, Stampfer MJ, et al. Vasectomy and Risk of Aggressive Prostate Cancer: A 24-Year Follow-Up Study. J Clin Oncol. 2014 Jul 7.
36. Weintraub S, Fahey C, Johnson N, Mesulam MM, Gitelman DR, Weitner BB, Rademaker A. Cogn Behav Neurol. Dec 2006; 19(4); 190-3.
37. Kahlenborn C. Breast Cancer, Its Link to Abortion and the Birth Control Pill. Dayton, OH: One More Soul; 2000: 12, 226.
38. Ryder RE. “Natural Family Planning”: Effective birth control supported by the Catholic Church. BMJ. 1993; 307: 723-726.
39. Kippley JF, Kippley SK. The Art of Natural Family Planning (Fourth Edition). The Couple to Couple League. 2007; 245.
The connection between contraception and abortion
Many in the pro-life movement are reluctant to make a connection between contraception and abortion. They insist that these are two very different acts–that there is all the difference in the world between contraception, which prevents a life from coming to be and abortion, which takes a life that has already begun.
With some contraceptives there is not only a link with abortion, there is an identity. Some contraceptives are abortifacients; they work by causing early term abortions. The IUD seems to prevent a fertilized egg–a new little human being- from implanting in the uterine wall. The pill does not always stop ovulation, but sometimes prevents implantation of the growing embryo. And, of course, the new RU-486 pill works altogether by aborting a new fetus, a new baby. Although some in the pro-life movement occasionally speak out against the contraceptives that are abortifacients, most generally steer clear of the issue of contraception. (more…)
Breast Cancer Risk from Abortion
How could abortion cause breast cancer?
At the beginning of pregnancy there are great increases in certain hormone levels (e.g., estrogen, progesterone, and hCG) that support pregnancy. In response to these changes, breast cells divide and mature into cells able to produce milk. Abortion causes an abrupt fall in hormone levels, leaving the breast cells in an immature state. These immature cells can more easily become cancer cells.1
Has this been proven? (more…)
Breast Cancer, Abortion, and the Pill
For the past year, One More Soul has been privileged to work with Dr. Chris Kahlenborn in publishing his new book: Breast Cancer, Its Link to Abortion and the Birth Control Pill . This book is the culmination of seven years the author spent reviewing and analyzing more than 500 research studies and related works. It is very timely because of the breast cancer epidemic, which currently threatens every woman.
In the concluding chapter of Dr. Kahlenborn’s book, he summarizes his conclusions and provides recommendations for action. The substance of that chapter is presented here, modified slightly to improve readability as a separate article. (more…)
The Hurtful Consequences of Artificial Contraception and Sterilization: Three Personal Testimonies
Rick and Peggy
In 1971, my husband and I were married. Thinking birth control must be okay because no one had said anything against it during my high school years and I had never heard a homily addressing the issue, I made an appointment with my family doctor. I asked if I needed to be on a stronger birth control pill, since now I would be taking it for the purpose of birth control instead of acne. He prescribed the pill and off I went.
We used contraceptives for the next three years. Our lives became very selfish and self-centered, as they caused us to become very empty and lonely. We thought, “There is more to life than this.” We had a strong yearning to have a baby and thought this was the right time. (more…)
The Challenge of Contraception for those who respect life
Contraception poses a challenge to those who respect life. It may not be immediately obvious that there is any connection between contraception and abortion, but on further examination, a relationship between the two becomes apparent. Ignoring the issue of contraception leads to a lost opportunity to respect life to the fullest degree. There are at least three connections between contraception and abortion to consider:
1. Many contraceptives can directly cause early abortions.
2. Contraceptive use creates a perceived need for abortion as a “back-up.”
3. Contraceptive use causes a devaluation of human life.
We’ll explore each of these ideas in the sections that follow. (more…)
The Harms of Contraception
There are several reasons why we believe that the use of contraception harms everyone involved. The first reason is that the use of contraception leads to abortion. Several “contraceptives” are in fact abortifacients. That is, they cause early abortions. All oral contraceptives, Norplant, Depo-Provera, and IUDs cause abortions before a woman even knows she’s pregnant. According to Dr. Bogomir Kuhar, in Infant Homicides Through Contraceptives, these forms of birth control take an estimated 8.1 to 12.75 million lives each year in the US alone. Contraceptives also cause abortions through their failures. All contraceptives fail, some quite often. Even surgical sterilization has a failure rate. Each “failure” results in a new human life, a new baby, an actual woman facing an unplanned and often unwanted pregnancy. These pregnancies are at risk for abortion. (more…)
How the Pill and Other Contraceptives Work
The birth control pill is currently being used by more than 10 million women in the US.1 A number of physicians and researchers have claimed that the birth control pill (BCP) (also called an oral contraceptive) is actually an abortifacient. An abortifacient is a substance that causes an abortion, the death of the zygote, embryo or fetus after conception has occurred. Others do not believe the BCP is an abortifacient as noted in a 1998 publication authored by several physicians: Hormonal Contraceptives: Are they Abortifacients? 2
This booklet uses an easy-reading question and answer format to review the available evidence for determining how the BCP works. All of that evidence, whether microscopic, macroscopic, or immunological, indicates that the BCP sometimes causes an early abortion. When and how often this happens remain unknown. (more…)
Intrauterine Devices (IUD/IUS): What Every Woman Needs to Know
What is an IUD?
An Intrauterine Device (IUD) is a small object that is placed inside a woman’s uterus (womb) for the purpose of preventing or interrupting pregnancy.
Currently, there are two kinds of IUDs available in the United States: the Copper-T IUD, made from plastic and copper, and the Intrauterine System IUS, a plastic device that releases hormones.
Is an IUD 100% effective?
No. Thecopper-T IUD has a clinical pregnancy rate of less than 1 per 100 women each year,1 and the IUS has a rate of 0.2 per 100 women each year.2 (more…)
The Pill and Breast Cancer
1) How could the Pill cause breast cancer?
Two of the most important types of hormones that control reproduction are estrogens and progestins. Birth control pills are made from synthetic estrogens and/or progestins. Experiments have shown that these hormones cause women’s breast cells to divide more rapidly.1 Cells that divide more rapidly are more prone to develop into cancer cells.
2) What is the evidence that the Pill and breast cancer are connected?
In 2005, the World Health Organization classified oral contraceptives as a Group I carcinogen—the most dangerous classification known.2 Also, a comprehensive meta-analysis3 published in the Mayo Clinic Proceedings in October 2006 found that 21 out of 23 retrospective studies done since 1980 showed that women who took oral contraceptives prior to the birth of their first child sustained a 44% average increased risk of developing pre-menopausal breast cancer (see research chart inside). This risk rose to 52% for women who took the Pill for at least four years prior to the birth of their first child.
3) How serious of a problem is breast cancer?
El cáncer de seno es la segunda causa más común de muerte por cáncer en las mujeres en los Estados
Unidos. Cerca de una en cada ocho mujeres desarrollará el cáncer de seno en alguna época en
su vida. En los EE.UU. cerca de 287.850 mujeres son diagnosticadas anualmente con cancer de
seno invasivo. y más de 43.000 mueren de esta enfermedad.4 La mitad de las mujeres que desarrollan el cáncer de seno tienen 62 años de edad o menos cuando se les realiza el diagnostico. Este riesgo es aun más alto cuando es combinado con otros factores de riesgo del cáncer de seno como el aborto inducido, el tratamiento con hormonas (tal como remplazo de estrógeno), la historia familiar del cáncer de seno, y otros.
4) Do some contraceptives cause more risk than others?
Yes. Research studies show that breast cancer risk is almost tripled for women who used Depo-Provera for 3 years or more before age 25.5
5) Are other types of cancer affected by oral contraceptive pills?
Oral contraceptives decrease the risk of ovarian and uterine cancer, while they increase the risk of liver, cervical and breast cancer.6 Since breast cancer is far more prevalent than the other three types of gynecological cancers, the Pill’s overall effect is detrimental to women.
6) Are there other risks from contraceptives?
Yes. Well known side effects of the Pill include an increased frequency of blood clots, high blood pressure, and heart attacks, as well as migraines, depression, loss of libido, and a variety of other disorders. Less well known is that oral contraceptives and injectable progestins (such as Depo-Provera) significantly increase the risk of contracting and transmitting HIV (the AIDS virus).7,8 In addition, medical studies strongly suggest that oral contraceptives work at times by causing an early abortion.9
7) How can I protect myself?
Many of the known risk factors for breast cancer can be avoided, such as hormone exposure (including hormonal contraceptives), induced abortion, heavy alcohol use, obesity, and radiation exposure. In addition, there is a significant reduction of risk with each child a woman bears. Every month of breastfeeding reduces breast cancer risk, as does bearing a child at a younger age. Some medications (e.g., raloxifene), which are taken after menopause to help strengthen bones, have been shown to markedly reduce the risk of post-menopausal breast cancer and should be considered by all women at high risk.10
8) If hormonal contraceptives are so dangerous, what options do couples have?
Natural Family Planning (NFP) methods are available and do not require chemicals or surgery and cause no increase in breast cancer risk. Not to be confused with the “rhythm method,” NFP is based primarily on observations of a woman’s cervical mucus. One of the largest research studies of NFP (involving 19,843 women and performed in India by the World Health Organization) showed a pregnancy rate of 0.2 pregnancies per 100 women yearly.11
Natural Family Planning methods have been used to diagnose and treat a variety of female reproductive disorders including infertility. Various medical problems (e.g., excessive menstrual cramping and bleeding), which are sometimes treated with contraceptive hormones, can often be treated by giving magnesium/calcium supplements and ibuprofen products after the onset of menses.
9) How can I find out more about breast cancer risk from the Pill?
Anyone may download the entire Mayo Clinic meta-analysis article by going to The Polycarp Research Institute (TPRI): Oral Contraceptive Use as a Risk Factor for Premenopausal Breast Cancer (TPRI) .In addition, eleven of the seventeen chapters in the book Breast Cancer, Its Link to Abortion and the Birth Control Pill deal with cancer risks from birth control pills.6
10) Where can I find information about Natural Family Planning?
Natural Family Planning information is available from a number of national organizations:
Billings Ovulation Method Association
www.Boma-usa.org (651) 699-8139
Liga de Pareja a Pareja
www.ligadepareja.org (800) 214-6028
FertilityCare Centers of America
www.fertilitycare.org (402) 505-8917
Fundación Familia de las Americas
www.familyplanning.net (301) 627-3346
Marquette Institute for Natural Family Planning
www.mu.edu/nursing/natural-family-planning.php
Natural Family Planning International
www.NFPandmore.org
SymptoPro
www.symptopro.org (971) 280-9676
US Conference of Catholic Bishops
www.usccb.org (202) 541-3240
One More Soul (Un Alma Más)
www.OneMoreSoul.com (800) 307-7685
Many Catholic dioceses have NFP offices or Family Life offices that can supply NFP information. Local parishes and Catholic hospitals may also be good sources.
References
1. Anderson T, Battersby S, et al. Oral contraceptive use influences resting breast proliferation. Hum Pathol. 1989; 20: 1139-1144.
2. World Health Organization International Agency for Research on Cancer. IARC Monographs. July 29, 2005.
3. Kahlenborn C, Modugno FM, et al. Oral contraceptive use as a risk factor for premenopausal breast cancer: a meta-analysis. Mayo Clin Proc. 2006; 81(10): 1290-1302.
4. American Cancer Society. Key Statistics for Breast cancer. Last revised: January 12, 2022. Retrieved from Breast Cancer Statistics | How Common Is Breast Cancer
5. Skegg DCG, Noonan EA, et al. Depot medroxyprogesterone acetate and breast cancer [A pooled analysis of the World Health Organization and New Zealand studies]. JAMA. 1995: 799-804.
6. Kahlenborn C. Breast Cancer, Its Link to Abortion and the Birth Control Pill. One More Soul, Dayton, 2000. Can be read or downloaded at www.onemoresoul.com/featured/breast-cancer-its-link-to-abortion-and-the-birth-control-pill.html.
7. Ungchusak, et al. Determinants of HIV infection among female commercial sex workers in northern Thailand: results from a longitudinal study. J Ac Immune Defic Syn Hum Retro. 1996. 12: 500-507.
8. Mostad SB, et al. Hormonal contraception, vitamin A deficiency and other risk factors for shedding HIV-1 infected cells from the cervix and the vagina. The Lancet 1997. 350: 922-927
9. Larimore WL, Stanford J. Postfertilization effects of oral contraceptives and their relationship to informed consent. Arch Fam Med. 9; 2000: 126-133
10. National Cancer Institute. Study of Tamoxifen and raloxifene (STAR) trial. April 26, 2006. (www.cancer.gov/star)
11. Ryder RE. “Natural Family Planning”: Effective birth control supported by the Catholic Church. Brit Med J. 1993; 307: 723-726.
Dr. Chris Kahlenborn practices Internal Medicine in Camp Hill, Pennsylvania, and is the current president of the Polycarp Research Institute (www.polycarp.org). He is the author of Breast Cancer, Its Link to Abortion and the Birth Control Pill, on which this pamphlet is partially based. This book (BBCL) is available from One More Soul at (800) 307-7685 for a suggested donation of $9.95 for the soft cover edition and $12.95 for the hardback, and can be read at www.OMSoul.com.
Breast Cancer, Its Link to Abortion and the Birth Control Pill is available from One More Soul at (800) 307-7685 for a suggested donation of $5.95 for the soft cover edition and $13.95 for the hardback.
More resources from Dr. Kahlenborn available at One More Soul
Breast Cancer: Abortion and the Pill
This booklet presents the summary, conclusions, and recommendations from Chapter 17 of the book Breast Cancer, Its Link to Abortion and the Birth Control Pill. A great resource for explaining just how dangerous abortion and contraceptive pills are. KBCL $1.00
Breast Cancer Risk from Abortion
Information from the book Breast Cancer, Its Link to Abortion and the Birth Control Pill, presented in a short and highly persuasive format. We have received letters and phone calls about babies saved from abortion when their mothers read this pamphlet. PBCA $0.35
The “Morning After Pill” and other types of “Emergency Contraception” – Myths and Realities
What is “emergency contraception”?
“Emergency contraception” is the use of a drug or a device after intercourse to prevent pregnancy. Emergency contraception is promoted for use when a woman has been raped, when a couple has chosen to have intercourse without using any form of contra-ception, or when there is a suspected contraceptive failure. Types of emergency contraception include the Morning After Pill, the insertion of the copper-T Intrauterine Device (IUD) five to seven days after intercourse, or the use of the abortion drugs Danazol or Mifepristone (RU-486).
What is the “Morning After Pill”? (more…)
Problems associated with Hormonal Birth Control
Health Problems associated with
Hormonal Birth Control
by
Dr. Rebecca Peck
Dr. Benjamin Peck
Fr. Juan R. Vélez, former MD
Updated by Liliana Cote de Bejarano, MD, MPH
Oral birth control (and all other hormonal birth control—HBC) is typically used to prevent pregnancy but is sometimes prescribed for other medical conditions. HBC causes many potential adverse effects: medical, social and spiritual. The vast majority of HBC prescriptions are given by physicians to healthy women, including adolescents with no known disease. Some women are prescribed hormonal birth control for only one reason—to prevent the completely normal condition of pregnancy.
Since all medications have potentially unwanted side effects, some of them serious, it is important that a physician weigh the risks and benefits when prescribing any medication. It follows that it is unethical to expose healthy women to health risks in order to prevent a normal condition. The mistake of exposing women to these risks is quite grave since other methods of family planning exist, like Natural Family Planning (NFP), which have no side effects.
As physicians, we do not prescribe hormonal birth control. The medical reasons for this decision are as follows:
HBC Treats Women’s Fertility and
Childbearing as a Disease
Although there can be legitimate medical and personal reasons for avoiding pregnancy, female fertility and the possibility of pregnancy itself are not diseases, and therefore do not need a pill (or patch, shot, IUD) for “treatment.”
HBC Causes Abortion
When HBC fails to suppress ovulation and other mechanisms of action that impede fertilization in a sexually active woman, conception may occur. HBC interferes with the implantation of a new human being by reducing the thickness of the lining of the uterus and altering implantation molecules and factors.1
Typical low dose HBC formulations only prevent the release of the female egg in about 65-75% of cycles.2,3
For this reason, if a woman has intercourse in her fertile phase, pregnancy and subsequent chemical abortion is possible in approximately 30% of the cycles.
HBC Contributes to an
Anti-Life Mentality
HBC (whether the Pill, patch, IUD or Shot) underpins the practice of abortion. People unwittingly conclude: “If birth control fails, abortion is the solution.” A nation-wide survey indicated that 54% of the women who had an abortion were using birth control the month before.4
HBC Increases the Risk of
Breast Cancer
Women face an increased risk of developing breast cancer while taking HBC and for at least ten years after the use of HBC is stopped. According to a study published in The New England Journal of Medicine using hormonal contraception for 10 years increases the risk of breast cancer by 38%. Additionally, the study showed that IUDs that release hormones also increase the risk for breast cancer.5 If the Pill is taken for four years before a woman’s first pregnancy, there is a 52% increased risk of breast cancer.6 An analysis of multiple studies noted that 21 out of 23 retrospective studies showed an increased risk of premenopausal breast cancer in women who took oral contraceptives prior to the birth of their first child.7
HBC Increases the Risk of
Blood Clots
A study of 1524 patients in the Netherlands concluded that hormonal contraceptives increased the risk of venous thrombosis fivefold compared with non-use.8 The risk is highest for HBC-using women who are overweight, smoke or are over 35 years of age.9
A recent systematic review reported that the use of combined oral contraceptives increased the risk of venous thrombosis fourfold compared to women who never used oral contraceptives.10
HBC increases the Risk of Suicide and Causes Changes in Healthy Body Metabolism
The study of almost half a million Danish women (2017) followed on average of 8.3 years concluded
that there was almost a twofold increased risk of suicide attempts in women using HBC. Also, there was a threefold increase in the risk of suicide in women using HBC compared to women who never use contraception.11 A recent study reported that the use of oral, vaginal, or transdermal HBC induced an increase in markers of chronic inflammation, a risk factor for cardiovascular disease. The use of combined contraceptives also impairs insulin sensitivity in young healthy women, which is a risk factor for diabetes mellitus.12 Additionally, HBC can produce migraine headaches, weight increase, moodiness, and loss of libido. It contributes to early increased bone loss.13The use of HBC is associated with infertility after prolonged use, and even to some extent with short-term use.
HBC Increases the Incidence of
Reproductive Organ Cancer
The use of HBC is associated with a significant increase in cancer of the cervix.14 It is likely that this follows infection with Human Papilloma Virus (HPV) which is a sexually transmitted infection.
HBC Increases the Risk of
Liver Tumors
There is some evidence that oral birth control increases the risk of certain benign and malignant liver tumors.15
HBC Increases the Risk of
Heart Attacks
First and second-generation oral birth control formulations have been linked to an increased risk of heart attacks (myocardial infarctions) and ischemic strokes.16 Third-generation oral birth control pills are associated with an increased risk of ischemic stroke.17 A 2015 analysis of multiple studies showed that women using combined oral contraceptive pills have a 1.6-fold increased risk to suffer heart attack or stroke.18
Harmful Effects of HBC on
Marriage and Society
Hormonal birth control fosters the mentality that men and women are incapable of self-control and are thus not able to abstain from sexual intercourse. The introduction of HBC was the catalyst for the sexual revolution with dramatic increases in premarital sex, adultery, divorce, abortion, and out-of-wedlock births. HBC has played an indirect role in the dramatic increase in single-parent families, poverty, and associated social ills in the U.S.19,20
Natural Family Planning (NFP) is an excellent way to plan your family
NFP is free of harmful side effects to women and families, and when used for just and serious reasons, can be very good for married couples. 21
References
- Klipping, C., Duijkers, I., Fortier, M. P., Marr, J., Trummer, D., & Elliesen, J. (2012). Long-term tolerability of ethinylestradiol 20 mug/drospirenone 3 mg in a flexible extended regimen: Results from a randomised, controlled, multicentre study.The Journal of Family Planning and Reproductive Health Care, 38(2), 84-93. doi:10.1136/jfprhc-2011-100214 [doi]
- Chowdhury, V., Joshi, U. M., Gopalkrishna, K., Betrabet, S., Mehta, S., & Saxena, B. N. (1980). ‘Escape’ ovulation in women due to the missing of low dose combination oral contraceptive pills.Contraception, 22(3), 241-247. doi:S0010-7824(80)80003-5 [pii]
- Baerwald AR, et al. Effects of oral contraceptives administered at defined stages of ovarian follicular development. Fertil Steril. 2006 Jul; 86(1): 27-35. Epub 2006 Jun 9.
- Jones, RK ,et al. Contraceptive use among U.S. women having abortions in 2000-2001. Perspec Sex Reprod Health. 2002; 34(6): 294-303.
- Morch, L. S., Skovlund, C. W., Hannaford, P. C., Iversen, L., Fielding, S., & Lidegaard, O. (2017). Contemporary hormonal contraception and the risk of breast cancer.The New England Journal of Medicine, 377(23), 2228-2239. doi:10.1056/NEJMoa1700732 [doi]
- Kahlenborn C. Breast Cancer, Its Link to Abortion and the Birth Control Pill. 2000.
- Kahlenborn, C., Modugno, F., Potter, D. M., & Severs, W. B. (2006). Oral contraceptive use as a risk factor for premenopausal breast cancer: A meta-analysis.Mayo Clinic Proceedings, 81(10), 1290-1302. doi:S0025-6196(11)61152-X [pii]
- van Hylckama Vlieg, A., Helmerhorst, F. M., Vandenbroucke, J. P., Doggen, C. J., & Rosendaal, F. R. (2009). The venous thrombotic risk of oral contraceptives, effects of oestrogen dose and progestogen type: Results of the MEGA case-control study.BMJ (Clinical Research Ed.), 339, b2921. doi:10.1136/bmj.b2921 [doi]
- Poulter, N. R. (2000). Risk of fatal pulmonary embolism with oral contraceptives.Lancet (London, England), 355(9221), 2088-6736(00)02369-2. doi:S0140-6736(00)02369-2 [pii]
- de Bastos, M., Stegeman, B. H., Rosendaal, F. R., Van Hylckama Vlieg, A., Helmerhorst, F. M., Stijnen, T., & Dekkers, O. M. (2014). Combined oral contraceptives: Venous thrombosis.The Cochrane Database of Systematic Reviews, (3):CD010813. doi(3), CD010813. doi:10.1002/14651858.CD010813.pub2 [doi]
- Skovlund, C. W., Morch, L. S., Kessing, L. V., Lange, T., & Lidegaard, O. (2018). Association of hormonal contraception with suicide attempts and suicides.The American Journal of Psychiatry, 175(4), 336-342. doi:10.1176/appi.ajp.2017.17060616 [doi]
- Piltonen, T., Puurunen, J., Hedberg, P., Ruokonen, A., Mutt, S. J., Herzig, K. H.,…Tapanainen, J. S. (2012). Oral, transdermal and vaginal combined contraceptives induce an increase in markers of chronic inflammation and impair insulin sensitivity in young healthy normal-weight women: A randomized study. Human Reproduction (Oxford, England), 27(10), 3046-3056.
- Wooltorton, E. (2005). Medroxyprogesterone acetate (depo-provera) and bone mineral density loss.CMAJ : Canadian Medical Association Journal = Journal De l’Association Medicale Canadienne, 172(6), 746. doi:cmaj.050158 [pii]
- La Vecchia, C., & Boccia, S. (2014). Oral contraceptives, human papillomavirus and cervical cancer.European Journal of Cancer Prevention: The Official Journal of the European Cancer Prevention Organisation (ECP), 23(2), 110-112. doi:10.1097/CEJ.0000000000000000 [doi]
- Giannitrapani, L., Soresi, M., La Spada, E., Cervello, M., D’Alessandro, N., & Montalto, G. (2006). Sex hormones and risk of liver tumor.Annals of the New York Academy of Sciences, 1089, 228-236. doi:1089/1/228 [pii]
- Tanis, B. C., van den Bosch, M. A., Kemmeren, J. M., Cats, V. M., Helmerhorst, F. M., Algra, A., . . . Rosendaal, F. R. (2001). Oral contraceptives and the risk of myocardial infarction.The New England Journal of Medicine, 345(25), 1787-1793. doi:10.1056/NEJMoa003216 [doi]
- Baillargeon, J. P., McClish, D. K., Essah, P. A., & Nestler, J. E. (2005). Association between the current use of low-dose oral contraceptives and cardiovascular arterial disease: A meta-analysis.The Journal of Clinical Endocrinology and Metabolism, 90(7), 3863-3870. doi:jc.2004-1958 [pii]
- Roach, R. E., Helmerhorst, F. M., Lijfering, W. M., Stijnen, T., Algra, A., & Dekkers, O. M. (2015). Combined oral contraceptives: The risk of myocardial infarction and ischemic stroke.The Cochrane Database of Systematic Reviews, (8):CD011054. doi(8), CD011054. doi:10.1002/14651858.CD011054.pub2 [doi]
- Akerlof, GA, et al. An analysis of out-of-wedlock childbearing in the United States. Q J Econ. 1996 May; 111(2):277-317.
- Akerlof, GA. Men without children. Econ J. 1998 Mar; 108(447): 287-309.
- Fehring, R. J. (2015). The influence of contraception, abortion, and natural family planning on divorce rates as found in the 2006-2010 national survey of family growth.The Linacre Quarterly, 82(3), 273-282. doi:10.1179/2050854915Y.0000000007 [doi]
Where can you learn more about
Natural Family Planning?
Billings Ovulation Method Association-USA
(888) 637-6371 www.Boma-usa.org
Couple to Couple League
(800) 745-8252 www.ccli.org
Family of the Americas Foundation
(800) 443-3395 www.familyplanning.net
FertilityCare Centers of America
(402) 390-6600, ext. 117 www.fertilitycare.org
Marquette Model
(414) 288-3854 www.NFP.Marquette.edu
Natural Family Planning International
(361-384-0067) www.NFPandmore.org
Northwest Family Services
(503) 215-6377 www.nwfs.org
US Conference of Catholic Bishops
(202) 541-3240 www.usccb.org
One More Soul
(800) 307-7685 www.OneMoreSoul.com

Problems Associated with Hormonal Birth Control
Four physicians who do not prescribe hormonal birth control give medical reasons for this decision.



Study: Abortion, Contraception Raise Breast Cancer Risk
Study is 9 months old, but still no warnings from cancer establishment
Contact: Karen Malec, Coalition on Abortion/Breast Cancer, 847-421-4000
MEDIA ADVISORY, Jan. 6 /Christian Newswire/ — Less than two months since the U.S. Preventative Services Task Force issued new guidelines recommending against routine mammograms for women in their forties, a second breast cancer scandal involving a U.S. government panel of experts has come to light which has implications for healthcare reform.
An April 2009 study by Jessica Dolle et al. of the Fred Hutchinson Cancer Research Center examining the relationship between oral contraceptives (OCs) and triple-negative breast cancer (TNBC) in women under age 45 contained an admission from U.S. National Cancer Institute (NCI) researcher Louise Brinton and her colleagues (including Janet Daling) that abortion raises breast cancer risk by 40%. [1]
Additionally, Dolle’s team showed that women who start OCs before age 18 multiply their risk of TNBC by 3.7 times and recent users of OCs within the last one to five years multiply their risk by 4.2 times. TNBC is an aggressive form of breast cancer associated with high mortality. (more…)
Posted in News & Commentary, Risks & Consequences | No Comments »